Learning Objectives
- Identify PPE types accurately.
- Demonstrate correct donning/doffing.
- Explain risk-based PPE selection.
- Describe proper disposal methods.
Prerequisite Knowledge
- Basic infection control principles.
- Understanding of transmission modes.
- Knowledge of hand hygiene.
Section 1: Types and Specifications of PPE
Deep Dive into PPE Categories
Personal Protective Equipment (PPE) comprises garments and devices designed to create a barrier between a healthcare worker and microbiological or chemical hazards. It is a fundamental component of Standard Precautions, which dictate that all patients are treated as potentially infectious. While administrative and engineering controls (e.g., ventilation, isolation rooms) are the primary lines of defense, PPE is the critical final barrier protecting the individual. Its effectiveness hinges not just on its presence, but on the correct selection of the specific type and material for the anticipated exposure (Siegel et al., 2007).
Gloves: The First Line of Contact Defense
Gloves are the most commonly used form of PPE in healthcare. Their primary function is twofold: to protect the hands of the healthcare worker from contamination with pathogens and to prevent the transfer of microorganisms from the worker's hands to patients or sterile equipment.
- Material Science: The choice of material is not arbitrary and has significant implications for protection and safety.
- Latex: Derived from natural rubber, latex gloves offer excellent elasticity, comfort, and tactile sensitivity. However, they pose a significant risk of Type I (immediate) and Type IV (delayed) hypersensitivity reactions in both workers and patients. Due to these allergy concerns, many institutions have transitioned to latex-free environments.
- Nitrile: A synthetic rubber, nitrile offers excellent resistance to chemicals, punctures, and a broad range of pathogens. It molds to the hand, providing good dexterity, and is the most common material used in clinical settings today. Its protein-free composition eliminates the risk of latex allergies.
- Vinyl (PVC): Polyvinyl chloride gloves are less expensive but offer a looser fit and are more permeable to certain microorganisms and chemicals. They are generally considered suitable only for low-risk, short-duration tasks that do not involve significant exposure to blood or body fluids.
- Sterile vs. Non-Sterile: Sterile gloves are required for invasive surgical procedures, insertion of central venous catheters, or any procedure that requires breaching sterile body cavities to prevent Surgical Site Infections (SSIs). Non-sterile, or "exam," gloves are used for all other patient care activities where contact with blood, body fluids, or contaminated surfaces is anticipated.
- Performance Metrics: Glove quality is assessed by the Acceptable Quality Level (AQL), an FDA-regulated standard that defines the maximum number of pinhole defects allowed in a batch. A lower AQL (e.g., 1.5) indicates a higher quality, more reliable barrier. Administrators should ensure that procured gloves meet the appropriate AQL for clinical use.
Gowns and Aprons: Protecting Skin and Clothing
Gowns and aprons are crucial for preventing the contamination of a healthcare worker's clothing and exposed skin, thereby limiting the potential for carrying pathogens out of a patient care area.
- AAMI Protection Levels: The Association for the Advancement of Medical Instrumentation (AAMI) provides a standardized classification system (ANSI/AAMI PB70) for gowns based on their ability to act as a barrier to liquids.
- Level 1: Minimal risk. Used for basic care, standard isolation, or as a cover gown for visitors. Provides a slight barrier to small amounts of fluid penetration.
- Level 2: Low risk. Used during blood draws or in the ICU. Tested for resistance to fluid penetration under constant contact and pressure.
- Level 3: Moderate risk. Used in the emergency room or during trauma cases where the potential for fluid spray or soakage is moderate. Provides a barrier against splatters.
- Level 4: High risk. Required for long, fluid-intense surgical procedures (e.g., orthopedic or cardiovascular surgery). These gowns are impervious to fluids and viral penetration for the duration of the procedure.
- Material and Design: Gowns are made from natural materials like cotton or synthetic nonwoven fabrics like Spunbond Meltblown Spunbond (SMS). The design is critical; effective gowns provide full coverage of the torso, fit comfortably over clothing, and have long sleeves that fit snugly at the wrist. The back is typically open, as it is considered a "clean" area less likely to be contaminated during patient care.
- Reusable vs. Disposable: The choice between reusable and disposable gowns involves a trade-off between environmental impact, long-term cost, and logistical complexity. Reusable gowns must undergo rigorous laundering and inspection processes to ensure their barrier integrity is maintained over multiple uses, which requires significant administrative oversight.
Respiratory Protection: Masks vs. Respirators
The distinction between surgical masks and respirators is one of the most critical and often misunderstood concepts in PPE. Their functions and protective capabilities are fundamentally different.
- Surgical/Procedure Masks: These are loose-fitting devices that create a physical barrier between the mouth and nose of the wearer and potential contaminants in the immediate environment. Their primary purpose is "source control"—to protect others from the wearer's respiratory emissions (droplets). They are not designed to create a tight seal against the face. ASTM International classifies these masks into three levels (1, 2, and 3) based on fluid resistance, filtration efficiency (for particles ≥3.0 microns), and breathability. They are effective against large-particle droplets but do not reliably protect the wearer from inhaling smaller airborne particles (aerosols).
- Respirators (e.g., N95): These are tight-fitting devices designed to filter airborne particles effectively. The "N95" designation means the respirator is not resistant to oil and filters at least 95% of airborne particles (down to 0.3 microns). Unlike masks, respirators rely on a tight facial seal to force inhaled air through the filter media. This is why they require mandatory annual fit-testing to ensure no air leaks around the edges. Their filtration mechanism is not a simple sieve; it involves a complex interplay of inertial impaction, interception, diffusion, and electrostatic attraction to capture particles far smaller than the filter's pore size. Respirators are essential for protecting the wearer from pathogens transmitted via the airborne route, such as Mycobacterium tuberculosis, measles virus, and SARS-CoV-2 during aerosol-generating procedures (World Health Organization, 2021).
Eye and Face Protection: Shielding Mucous Membranes
The mucous membranes of the eyes, nose, and mouth are vulnerable portals of entry for pathogens. Eye and face protection are designed to shield these areas from splashes, sprays, and spatter of blood or other potentially infectious materials.
- Goggles: Provide a tight seal around the eyes, offering excellent protection from splashes from all directions. Vented goggles help reduce fogging, but indirectly vented or non-vented types offer superior splash protection.
- Face Shields: A sheet of transparent plastic that covers the entire face. It protects the eyes, nose, and mouth. Face shields offer the advantage of covering a larger area and are often more comfortable for extended wear. They should extend from the chin to above the eyebrows and wrap around the sides of the face. They are typically worn in conjunction with a mask or respirator.
- Safety Glasses: While providing impact protection, standard safety glasses are inadequate for infection control as they do not seal around the eyes. Those with solid side shields offer some protection but are inferior to goggles or face shields for biological hazards. All eye protection used in healthcare should comply with ANSI Z87.1 standards for impact resistance and optical clarity.
Examples in Practice
- Gloves: A phlebotomist uses non-sterile nitrile gloves to draw a blood sample. For inserting a central line, a physician dons sterile latex-free gloves after performing a surgical scrub.
- Gown: A nurse caring for a patient with an active C. difficile infection wears a disposable, cuffed, Level 2 isolation gown. An orthopedic surgeon wears a sterile, fluid-impervious Level 4 surgical gown during a knee replacement surgery.
- Respirator vs. Mask: A healthcare provider wears a standard surgical mask when talking to a patient with a common cold. The same provider must wear a fit-tested N95 respirator before entering the room of a patient with suspected active pulmonary tuberculosis.
- Face Shield: An endoscopist wears a face shield over a surgical mask during a gastroscopy to protect against potential splashes of gastric contents.
Did You Know?
Plague doctors in 17th century Europe wore a special costume consisting of a bird-like beak mask containing aromatic herbs, an ankle-length overcoat, gloves, boots, a wide-brimmed hat, a linen hood, and an outer over-clothing garment.
Section 1 Summary
The selection of PPE is a clinical decision based on the specific task and anticipated level of exposure. The four main categories are gloves (nitrile, vinyl), gowns (AAMI Levels 1-4), respiratory protection (masks for source control, respirators for wearer protection), and eye/face protection (goggles, face shields). Understanding the material science, performance standards (e.g., AQL, ASTM, ANSI), and intended use of each item is essential for ensuring both healthcare worker and patient safety.
Reflective Questions
- How does the material of a glove, beyond just allergy potential, impact its protective capability and the user's dexterity during a delicate procedure?
- From a hospital administration perspective, what are the key factors to consider when deciding between a policy of using disposable vs. reusable Level 2 isolation gowns? Consider cost, logistics, environmental impact, and staff training.
- A patient presents with a cough and fever. The specific diagnosis is unknown. When would a surgical mask be considered sufficient protection, and what specific clinical signs would necessitate upgrading to an N95 respirator?
Section 2: Usage Protocol: Donning and Doffing
The Critical Science of Sequence
The most sophisticated, high-level PPE is rendered ineffective—and even dangerous—if not used correctly. The processes of putting on (donning) and, more importantly, taking off (doffing) PPE are structured, evidence-based sequences designed to minimize the risk of contamination. The fundamental principle guiding these protocols is that the exterior surfaces of PPE become contaminated during use. Doffing, therefore, is a high-risk procedure where self-contamination is most likely to occur. Studies utilizing fluorescent tracers have consistently shown that without rigorous training and adherence to protocol, healthcare workers frequently contaminate their skin and clothing during PPE removal (Bello et al., 2021).
Donning (Putting On) PPE: A Methodical Approach
The goal of donning is to apply PPE in a way that ensures full coverage and functionality before entering a contaminated environment or engaging in a clinical procedure. The sequence is logical, moving from the largest items to the smallest and ensuring a proper seal. Before beginning, it is critical to perform hand hygiene and ensure all necessary PPE is available and appropriately sized.
The most widely accepted sequence, recommended by the Centers for Disease Control and Prevention (CDC), is as follows:
- Gown:
- Select the appropriate size and type (e.g., isolation vs. surgical).
- Unfold the gown and slide both arms into the sleeves.
- Fasten the ties at the back of the neck first, then secure the ties at the waist. Ensure the gown fully covers the torso from neck to knees and the arms to the end of the wrists.
- Rationale: The gown forms the foundational barrier. Applying it first ensures that subsequent items (like masks and gloves) are layered over it correctly.
- Mask or Respirator:
- Secure the ties or elastic bands at the middle of the head and neck (for tie-on masks) or around the head (for elastic).
- Fit the flexible band to the bridge of the nose to create a close fit.
- For a respirator, ensure the bottom strap is below the ears and the top strap is above. Check the seal by inhaling and exhaling sharply (user seal check).
- Rationale: The mask/respirator must be in place before gloves are donned, as adjusting it with contaminated gloves would be a breach of protocol. A proper seal is paramount for respirators.
- Goggles or Face Shield:
- Place over the face and eyes and adjust to fit. The headband should be secure but comfortable.
- Ensure it does not interfere with the seal of the respirator, if worn.
- Rationale: This item protects the mucous membranes of the eyes and should be placed after the respirator to ensure it sits correctly.
- Gloves:
- Select the correct size. Gloves that are too small may tear, and those that are too large can compromise dexterity.
- Extend the gloves to cover the cuffs of the isolation gown completely. This creates a continuous, sealed barrier.
- Rationale: Gloves are donned last because they are the most likely item to be changed during a procedure and must form a seal over the gown. This is a critical step to prevent fluid from running up under the sleeve.
In high-risk settings, such as those for Ebola or other viral hemorrhagic fevers, a "buddy system" where a trained observer supervises the donning process is considered best practice to catch any errors.
Doffing (Taking Off) PPE: The Moment of Highest Risk
Doffing is the most critical and complex part of the PPE protocol. The sequence is designed to remove the most contaminated items first and to progress in a manner that avoids touching contaminated surfaces with bare hands or clean clothing. The guiding principle is to touch only "clean" inside surfaces when removing items. A designated doffing area, separate from the patient zone, is ideal. Hand hygiene is an integral part of the process, performed at key steps and immediately upon completion.
The standard CDC-recommended sequence is as follows:
- Gloves:
- This is the most contaminated item. Using one gloved hand, grasp the palm area of the other gloved hand and peel it off, turning it inside out.
- Hold the removed glove in the remaining gloved hand.
- Slide the fingers of the ungloved hand under the remaining glove at the wrist, taking care not to touch the outside surface.
- Peel this second glove off over the first glove, creating a small bag containing both gloves, and discard in the appropriate receptacle.
- Rationale: Removing gloves first eliminates the primary source of contamination from the hands, allowing for safer removal of other items.
- Goggles or Face Shield:
- Handle by the clean headband or earpieces from behind the head. Lift away from the face without touching the contaminated front surface.
- Place in a designated receptacle for disposal or reprocessing.
- Rationale: The front of the eye protection is considered highly contaminated. Removing from the back prevents transfer of pathogens to the hands.
- Gown:
- Untie the neck ties first, then the waist ties. Allow the gown to fall forward from the shoulders.
- Touching only the inside of the gown, pull it away from the body.
- As you remove it, fold or roll the gown into a bundle with the contaminated outside surface turned inward. Discard immediately.
- Rationale: This technique contains the contamination within the gown and prevents the outside from touching your scrubs or skin.
- Mask or Respirator:
- This is done last, just before exiting the room.
- Untie the bottom tie first, then the top tie (or grasp the bottom elastic, then the top). This prevents the mask from flipping down and contaminating your uniform.
- Remove the mask by handling only the ties/elastics and discard it. Do not touch the front of the mask.
- Rationale: The front of the mask is a filter and is considered contaminated. Removing it last ensures respiratory protection is maintained until you have left the immediate patient environment.
- Immediate Hand Hygiene:
- Immediately after removing all PPE and exiting the patient room, perform thorough hand hygiene using alcohol-based hand rub or soap and water.
- Rationale: This is the final, non-negotiable step to remove any contaminants that may have been transferred to the hands during the doffing process.
Examples in Practice
- Correct Donning Scenario: Before entering the room of a patient on droplet precautions for influenza, a nurse performs hand hygiene, ties on a gown, secures a surgical mask and face shield, and finally pulls gloves over the gown cuffs.
- Common Doffing Error: A clinician removes their gown by pulling it over their head, causing the contaminated outer surface to brush against their face and hair. The correct method is to peel it off from the shoulders, turning it inside out.
- High-Risk Doffing: After an aerosol-generating procedure, a respiratory therapist proceeds to a designated anteroom to doff. They remove gloves and gown together, then face shield, perform hand hygiene, exit the anteroom, and then remove their N95 respirator in a clean area, followed by final hand hygiene. This multi-step process with integrated hand hygiene minimizes contamination risk.
PPE Don and Doff Poster
Did You Know?
The origin of the modern surgical glove is a story of romance and necessity. In the late 1880s at Johns Hopkins Hospital, chief surgeon William Halsted was concerned that the harsh antiseptic solutions were causing severe dermatitis on the hands of his chief surgical nurse, Caroline Hampton (whom he would later marry). He commissioned the Goodyear Rubber Company to create thin, pliable rubber gloves she could wear. The gloves not only protected her hands but were soon adopted by Halsted and his team, who noted a dramatic decrease in post-operative infections, ushering in a new era of aseptic surgery.
Did You Know?
The 2014 Ebola virus outbreak in West Africa was a watershed moment for PPE protocols. Initial high rates of infection among healthcare workers prompted an intensive re-evaluation of doffing procedures by organizations like the CDC. This led to the development of more stringent, prescriptive, and visually-guided protocols, often requiring a trained observer to call out each step. This crisis underscored that the human factor—how PPE is used—is just as important as the equipment itself.
Section 2 Summary
Correct PPE usage is a procedural skill critical for infection prevention. The donning sequence (gown, mask/respirator, goggles/face shield, gloves) is designed to establish a complete barrier. The doffing sequence (gloves, goggles/face shield, gown, mask/respirator) is more critical and aims to prevent self-contamination by removing the most soiled items first and handling all equipment by its "clean" surfaces. Meticulous hand hygiene is required before donning and immediately after doffing to ensure safety.
Reflective Questions
- Why is the doffing sequence considered a higher-risk procedure than the donning sequence for healthcare worker safety? What are the specific points of failure?
- Consider the environmental factors in a busy, multi-patient hospital ward (e.g., limited space, interruptions, emergencies). How can hospital administrators design workflows and physical spaces to better support correct doffing procedures?
- Imagine you are training a new nursing graduate. How would you explain the rationale behind each step of the doffing sequence to help them understand the "why" and not just memorize the "how," especially for performance under pressure?
Section 3: Risk Assessment, Selection, and Proper Disposal
Beyond Rote Memory: A Framework for Clinical Decision-Making
Effective PPE use transcends memorizing sequences; it requires healthcare professionals to become proficient in dynamic risk assessment. The selection of appropriate PPE is not a "one-size-fits-all" directive but a clinical judgment based on a nuanced understanding of the pathogen, the patient, the environment, and the task at hand. This approach is encapsulated in the dual frameworks of Standard Precautions and Transmission-Based Precautions (Siegel et al., 2007).
The Hierarchy of Precautions
- Standard Precautions: This is the foundational level of infection control. It assumes that every patient is potentially infectious and that their blood and all body fluids (except sweat) may contain transmissible infectious agents. Standard Precautions apply to all patient care, in any healthcare setting. This includes hand hygiene, and the use of PPE—gloves, gowns, masks, eye protection—based on anticipated exposure. For example, a nurse will don gloves to draw blood from any patient, regardless of their known infection status.
- Transmission-Based Precautions: This is a second tier of precautions used in addition to Standard Precautions for patients who are known or suspected to be infected with pathogens that spread in specific ways. These precautions are tailored to the mode of transmission.
- Contact Precautions: Used for pathogens spread by direct or indirect contact (e.g., Methicillin-resistant Staphylococcus aureus (MRSA), C. difficile). PPE required: Gown and gloves for all interactions that may involve contact with the patient or potentially contaminated areas in the patient's environment.
- Droplet Precautions: Used for pathogens spread in large respiratory droplets generated by coughing, sneezing, or talking (e.g., influenza, pertussis). PPE required: Surgical mask worn upon entering the patient's room. Eye protection might be added based on risk of splashes.
- Airborne Precautions: Used for pathogens that remain infectious over long distances when suspended in the air as small aerosolized particles (e.g., tuberculosis, measles, varicella). PPE required: A fit-tested N95 or higher-level respirator. This also requires engineering controls, such as placing the patient in an airborne infection isolation room (AIIR) with negative pressure.
Pathogen Transmission Prevention Poster

Conducting a Point-of-Care Risk Assessment (PCRA)
Before any patient interaction, the healthcare worker must pause to conduct a mental PCRA. This involves asking four key questions:
- What is the nature of the patient interaction? Will it be a brief conversation, or will it involve prolonged, close contact and manipulation of body fluids (e.g., wound care, suctioning)?
- What is the likelihood of exposure to blood, body fluids, or an infectious agent? Is the patient coughing or sneezing? Do they have uncontrolled diarrhea or a draining wound? Is an aerosol-generating medical procedure (AGMP) planned?
- What is the patient's known or suspected infection status? Are they on Transmission-Based Precautions?
- What combination of PPE is required to prevent exposure? Based on the answers above, select the appropriate level of gown, type of respiratory protection, and need for eye shields.
This dynamic process empowers clinicians to adapt their PPE use to the specific situation, ensuring adequate protection without overuse, which is critical for resource stewardship (Government of Canada, 2022).
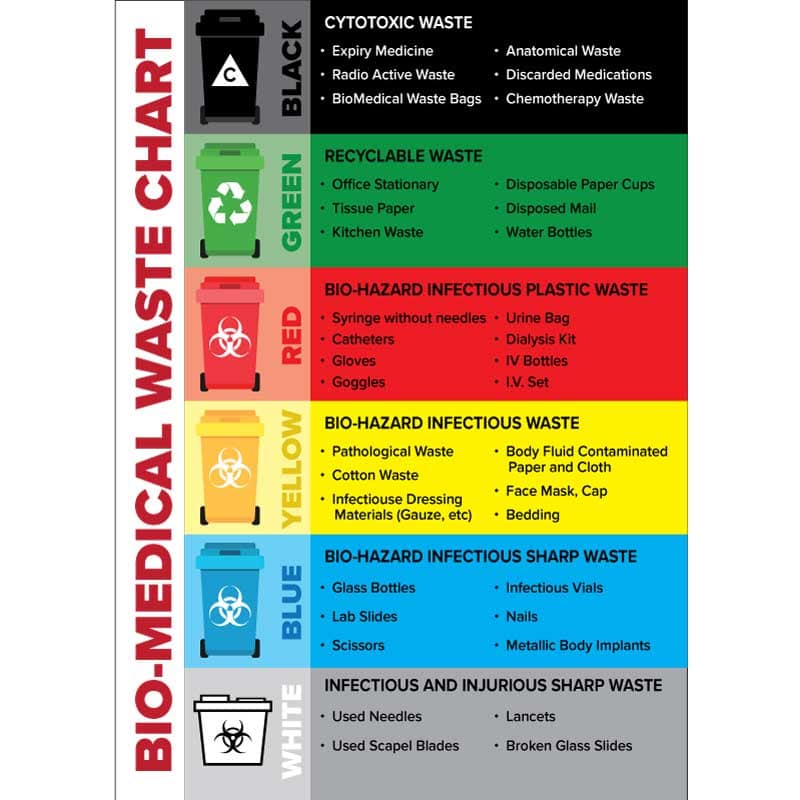
The Final Step: Proper Disposal and Waste Management
The life cycle of PPE does not end with its removal. Proper disposal is a crucial final step to prevent the spread of infection to other staff, patients, and the wider community, and to comply with strict environmental and occupational health regulations. Healthcare waste is segregated into different streams based on its potential hazard.
- Biohazardous (Regulated Medical) Waste: This stream is typically collected in red bags or specially marked containers. According to the Occupational Safety and Health Administration (OSHA), this includes items contaminated with liquid or semi-liquid blood or other potentially infectious materials (OPIM), and items that would release these materials if compressed. This means PPE that is saturated or dripping with blood, or heavily soiled with body fluids, must be disposed of as biohazardous waste.
- General (Non-Infectious) Waste: This stream is for standard municipal solid waste, collected in clear or black bags. PPE that is not visibly soiled, such as a mask worn for droplet precautions or gloves used for a routine patient assessment with no fluid contact, can typically be disposed of in the general waste stream. Policies may vary by institution and local regulations.
- Sharps Waste: While not PPE, it's critical to remember that sharps containers are exclusively for items that can puncture or cut skin (needles, scalpels, etc.). PPE must never be placed in a sharps container, as this can cause overfilling and create a significant injury risk.
From an administrative perspective, improper waste segregation has significant consequences. Over-classifying general waste as biohazardous is extremely costly, as its treatment (e.g., autoclaving, incineration) is far more expensive than landfill disposal. Conversely, under-classifying biohazardous waste poses a serious public health risk. Therefore, continuous staff education on waste segregation is a key component of a hospital's infection prevention and financial management strategy.
The Challenge of Sustainability
The COVID-19 pandemic brought the environmental impact of single-use PPE into sharp focus, generating an unprecedented amount of plastic waste (UNEP, 2020). This has spurred innovation in the field, including the development of reusable elastomeric respirators, improved protocols for decontaminating and reusing N95s in crisis capacity scenarios, and the creation of more effective, launderable isolation gowns. Hospital administrators must now navigate the complex balance between maintaining the highest standards of infection control, managing costs, ensuring a resilient supply chain, and promoting environmental stewardship. This may involve investing in high-quality reusable PPE programs and exploring partnerships with medical waste recycling companies.
Examples in Practice
- Risk Assessment Scenario: A respiratory therapist is called to intubate a patient with acute respiratory distress of unknown cause. This is a high-risk aerosol-generating procedure. The therapist's PCRA leads them to select an N95 respirator, a face shield, a Level 3 fluid-resistant gown, and double gloves.
- Waste Segregation Scenario: A nurse changes a heavily saturated dressing on a post-operative wound. The gloves and gown, visibly soiled with blood and exudate, are placed in the red biohazard bag. The paper wrapper from the new dressing is placed in the regular trash can.
- Administrative Decision: A hospital's infection control committee reviews its PPE purchasing. They decide to invest in a fleet of reusable Level 2 gowns and a commercial laundry service for non-critical care areas, projecting a 30% cost saving and significant waste reduction over three years, while maintaining disposable Level 4 gowns for surgical use.
Proper Waste Disposal Poster
Did You Know?
During the peak of the COVID-19 pandemic, the World Health Organization estimated a global monthly need of 89 million medical masks, 76 million examination gloves, and 1.6 million pairs of goggles. This massive surge in demand not only strained supply chains but also resulted in an estimated 75% of pandemic-associated plastic waste being mismanaged, ending up in landfills or oceans, highlighting the urgent need for sustainable healthcare waste solutions.
Section 3 Summary
Effective PPE strategy relies on a robust risk assessment framework, encompassing Standard and Transmission-Based Precautions. The Point-of-Care Risk Assessment (PCRA) empowers clinicians to select the correct PPE for each specific patient interaction. After use, PPE must be disposed of correctly. Visibly soiled items typically go into biohazardous waste, while non-soiled items may go into general waste, per institutional policy. Proper waste segregation is critical for safety, regulatory compliance, and cost control. The future of PPE management will increasingly involve balancing infection control with environmental sustainability.
Reflective Questions
- Describe a clinical scenario where Standard Precautions alone would be insufficient, detailing which Transmission-Based Precaution would be necessary and what specific PPE that entails.
- What are the potential downstream consequences—both financial and safety-related—for a hospital if its staff consistently dispose of all used PPE in biohazard bins, regardless of the level of contamination?
- As a hospital administrator, how would you design a program to promote a culture where correct, risk-based PPE selection and waste segregation become ingrained, second-nature behaviors for all clinical staff?
Glossary
- AAMI Levels
- A four-tiered classification system by the Association for the Advancement of Medical Instrumentation that rates the barrier protection of surgical gowns and drapes against fluid penetration.
- Donning
- The process of putting on Personal Protective Equipment in a specific sequence to ensure maximum protection.
- Doffing
- The process of taking off Personal Protective Equipment in a specific sequence to prevent self-contamination.
- N95 Respirator
- A type of respiratory protective device that fits tightly to the face and filters at least 95% of airborne particles. It requires fit-testing to be effective.
- Standard Precautions
- A set of infection control practices used to prevent transmission of diseases that can be acquired by contact with blood, body fluids, non-intact skin, and mucous membranes. Applied to all patients.
- Transmission-Based Precautions
- Additional infection control precautions used for patients known or suspected to be infected with pathogens that can be spread by airborne, droplet, or contact routes.
References
- Bello, A., Omololu, O., & Oduyebo, O. O. (2021). Simulation-based training on donning and doffing of personal protective equipment for healthcare workers in a low-resource setting. Journal of Educational and Health Promotion, 10, 185. https://doi.org/10.4103/jehp.jehp_1052_20
- Government of Canada. (2022). Routine practices and additional precautions for preventing the transmission of infection in healthcare settings. Public Health Agency of Canada. https://www.canada.ca/en/public-health/services/infectious-diseases/nosocomial-occupational-infections/routine-practices-additional-precautions-preventing-transmission-infection-healthcare-settings.html
- Siegel, J. D., Rhinehart, E., Jackson, M., Chiarello, L., & Health Care Infection Control Practices Advisory Committee. (2007). 2007 guideline for isolation precautions: Preventing transmission of infectious agents in health care settings. Centers for Disease Control and Prevention. https://www.cdc.gov/infectioncontrol/pdf/guidelines/isolation-guidelines-H.pdf
- United Nations Environment Programme (UNEP). (2020). Waste management an essential public service in the fight to beat COVID-19. https://www.unep.org/news-and-stories/story/waste-management-essential-public-service-fight-beat-covid-19
- World Health Organization. (2021). Infection prevention and control during health care when COVID-19 is suspected or confirmed. https://www.who.int/publications/i/item/WHO-2019-nCoV-IPC-2021.1