Isolation Protocols for Infectious Patients
Learning Objectives
- Understand isolation precaution types.
- Implement quarantine procedures effectively.
- Analyze air ventilation systems.
- Apply correct PPE protocols.
- Mitigate psychosocial patient impacts.
Prerequisite Knowledge
- Basic microbiology and pathogens.
- Understanding of transmission modes.
- Familiarity with PPE types.
Section 1: Patient Isolation Principles and Practices
Introduction: Breaking the Chain of Infection
Patient isolation is a cornerstone of infection prevention and control within any healthcare facility. It is not merely about separating a patient physically; it is a scientifically-grounded set of practices designed to interrupt the transmission of infectious agents. To understand its profound importance, we must revisit the chain of infection. This chain consists of six links: the infectious agent (pathogen), the reservoir (where the pathogen lives), the portal of exit, the mode of transmission, the portal of entry, and the susceptible host. Isolation protocols are primarily designed to sever the 'mode of transmission' link, thereby protecting other patients, healthcare workers, and visitors.
The decision to place a patient in isolation is a critical clinical judgment based on the suspected or confirmed infectious disease, the pathogen's mode of transmission, and the patient's specific circumstances. Failure to implement these protocols effectively can lead to healthcare-associated infections (HAIs), outbreaks, increased patient morbidity and mortality, and significant financial costs to the healthcare system (Siegel et al., 2007). This section provides a deep dive into the two tiers of precautions recommended by the Centers for Disease Control and Prevention (CDC) and other global health bodies: Standard Precautions and Transmission-Based Precautions.
Tier 1: Standard Precautions - The Universal Foundation
Standard Precautions are the minimum infection prevention practices that apply to all patient care, regardless of suspected or confirmed infection status, in any setting where healthcare is delivered. The core principle is that all blood, body fluids, secretions, excretions (except sweat), non-intact skin, and mucous membranes may contain transmissible infectious agents. Therefore, these precautions are a universal safeguard.
Key components of Standard Precautions include:
- Hand Hygiene: This is the single most important practice to reduce the transmission of infectious agents. It includes washing hands with soap and water or using an alcohol-based hand sanitizer before and after patient contact, after contact with potentially infectious material, and after removing gloves.
- Use of Personal Protective Equipment (PPE): This involves selecting and using appropriate PPE—such as gloves, gowns, masks, and eye protection—based on an assessment of risk for exposure to blood or body fluids. For example, gloves are worn when touching blood or body fluids, and a gown is added if splashing of these fluids is anticipated.
- Respiratory Hygiene and Cough Etiquette: This strategy is targeted at patients and accompanying individuals with respiratory symptoms. It includes covering the mouth and nose when coughing or sneezing, using tissues and disposing of them properly, and performing hand hygiene after contact with respiratory secretions.
- Safe Injection Practices: These practices are designed to prevent transmission of infectious diseases between patients, or between a patient and a healthcare provider, during the preparation and administration of parenteral medications. This includes using a new, sterile needle and syringe for every injection.
- Safe Handling of Potentially Contaminated Equipment or Surfaces: This involves cleaning and disinfecting medical equipment and the patient environment in a routine, standardized manner. Equipment used for patient care should be properly cleaned and reprocessed, and single-use items must be discarded correctly.
Adherence to Standard Precautions is not optional; it is the bedrock upon which all other infection control measures are built. It creates a baseline of safety that protects both the provider and the patient in every encounter.
Tier 2: Transmission-Based Precautions - A Targeted Approach
When Standard Precautions alone are insufficient to interrupt the transmission of a specific pathogen, Transmission-Based Precautions are implemented. These are used for patients who are known or suspected to be infected or colonized with infectious agents that require additional control measures to prevent transmission. These precautions are always used in addition to Standard Precautions. There are three main categories of Transmission-Based Precautions: Contact, Droplet, and Airborne.
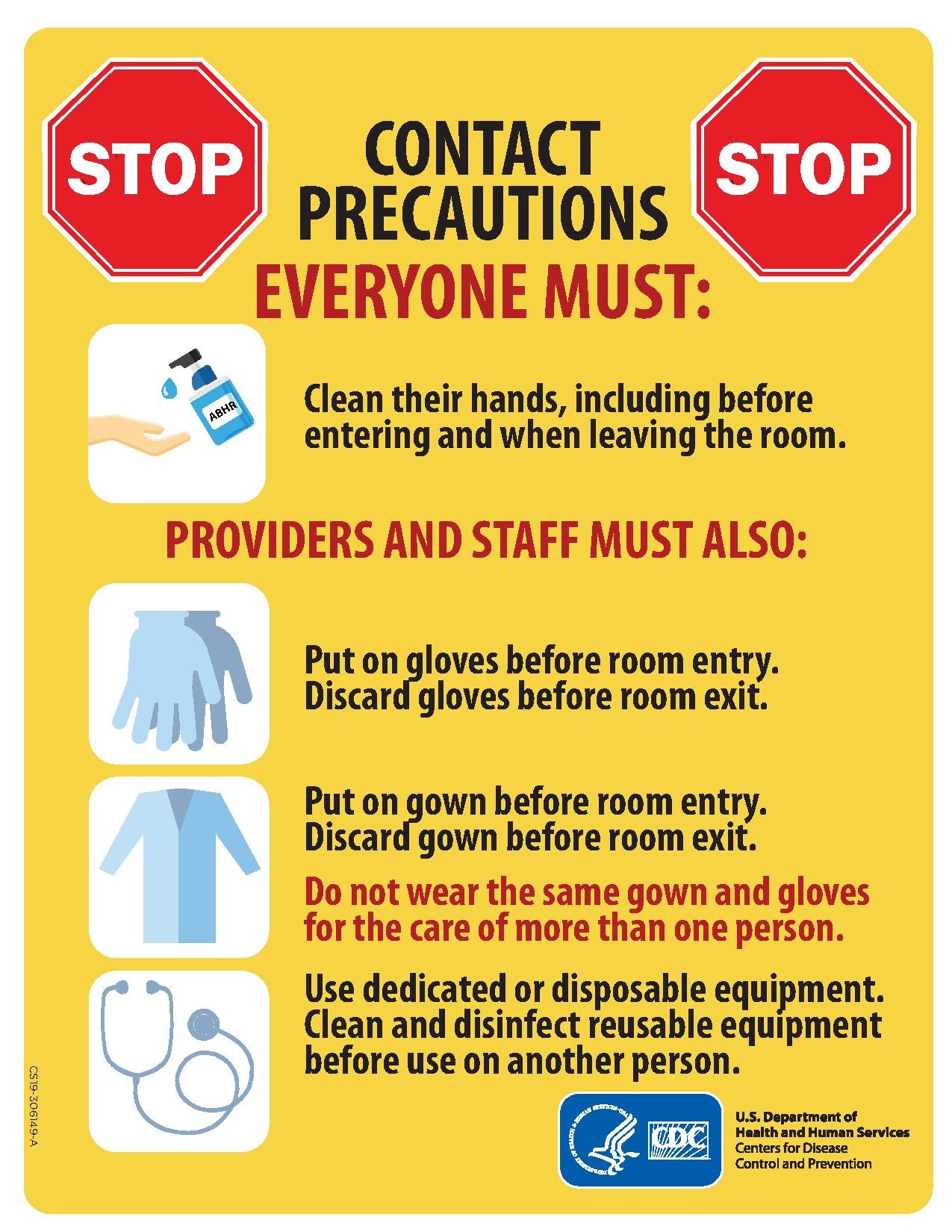
1. Contact Precautions
Rationale: Used for pathogens that spread through direct or indirect contact with the patient or the patient's environment. Direct contact involves skin-to-skin contact, while indirect contact involves touching a contaminated intermediate object (fomite), such as bed rails, medical equipment, or doorknobs.
Indications: Commonly used for infections like Methicillin-resistant Staphylococcus aureus (MRSA), Vancomycin-resistant Enterococci (VRE), Clostridioides difficile (C. diff), norovirus, and major draining wounds.
Core Requirements:
- Patient Placement: A single-patient room is preferred. If not available, cohorting (placing patients with the same infection in the same room) is an option. When cohorting, ensure patients are physically separated by more than 3 feet and have separate commodes and equipment.
- Personal Protective Equipment (PPE): Wear gloves upon entering the room. Wear a gown upon entering the room, especially if substantial contact with the patient or their environment is anticipated. Remove all PPE before exiting the room and perform hand hygiene immediately.
- Patient Transport: Limit the movement and transport of the patient from the room to medically necessary purposes only. Ensure infected or colonized areas of the patient's body are contained and covered.
- Equipment: Use disposable or dedicated non-critical patient-care equipment (e.g., blood pressure cuff, stethoscope). If equipment must be shared, it must be thoroughly cleaned and disinfected before use on another patient.
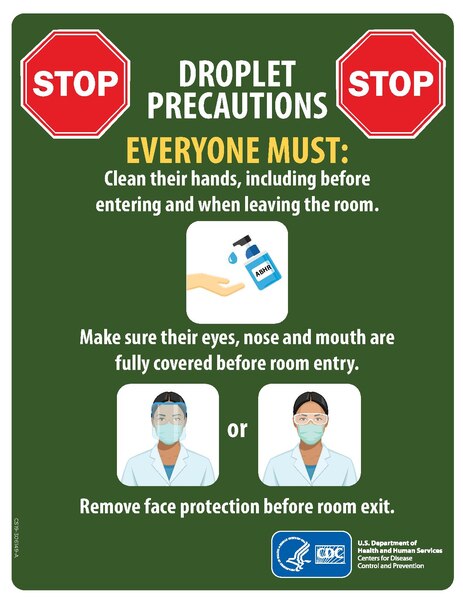
2. Droplet Precautions
Rationale: Used for pathogens transmitted by large respiratory droplets (>5 micrometers in diameter) generated by a patient who is coughing, sneezing, or talking. These droplets travel short distances (typically up to 6 feet) and do not remain suspended in the air. Transmission occurs when droplets are propelled and deposited on the host's conjunctivae, nasal mucosa, or mouth.
Indications: Influenza, pertussis (whooping cough), meningococcal disease, mumps, and rubella.
Core Requirements:
- Patient Placement: A single-patient room is preferred. If not available, cohort with a patient with the same active infection. If neither is possible, maintain spatial separation of at least 3-6 feet between the infected patient and other patients.
- Personal Protective Equipment (PPE): Wear a surgical mask upon entering the patient's room or when working within 6 feet of the patient. The use of gowns and gloves follows Standard Precautions, based on the risk of contact with body fluids.
- Patient Transport: Limit transport. If the patient must leave the room, they should wear a surgical mask and follow respiratory hygiene/cough etiquette.
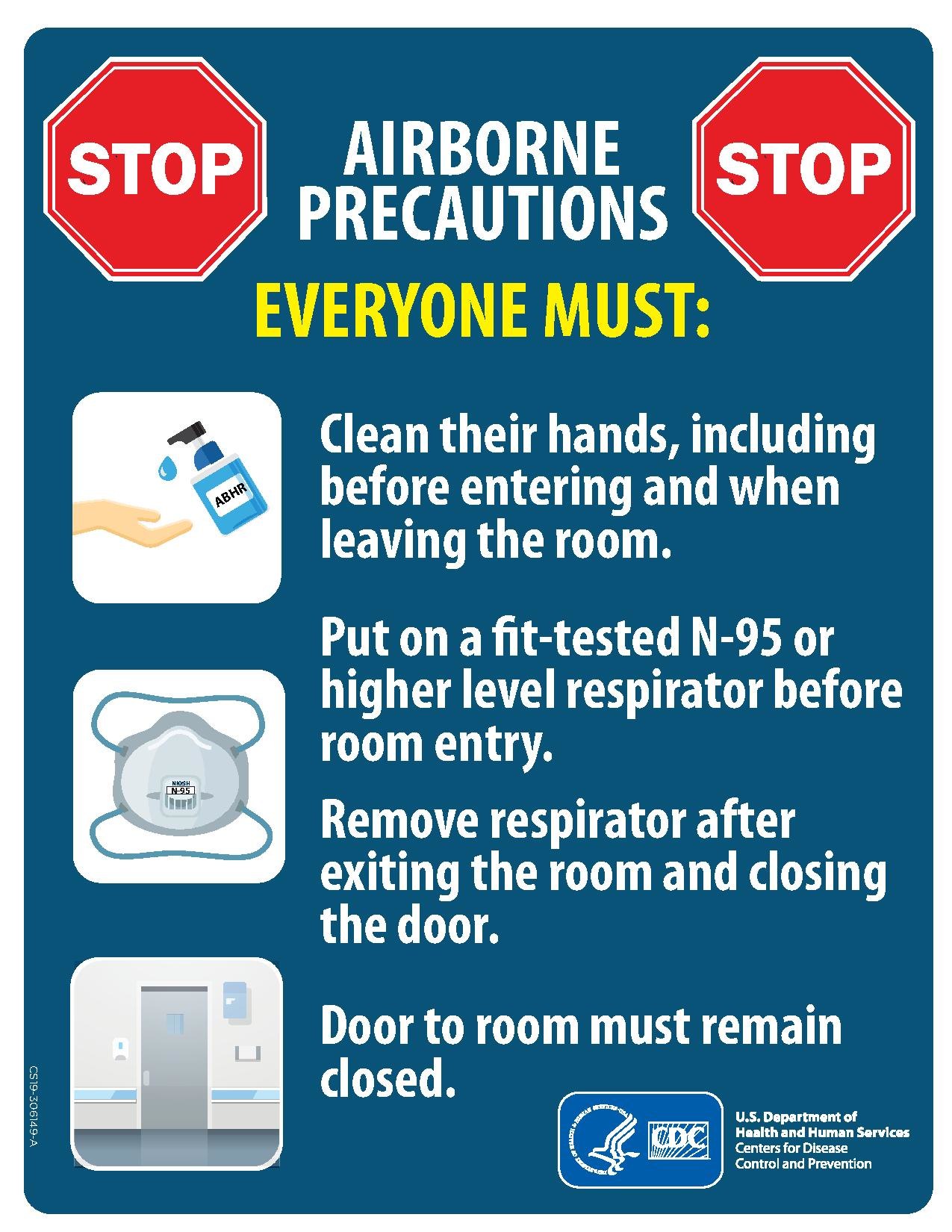
3. Airborne Precautions
Rationale: Used for pathogens transmitted by airborne droplet nuclei (particles <5 micrometers in diameter). These small particles can remain suspended in the air for long periods and can be dispersed over long distances by air currents. This is the most stringent level of precaution.
Indications: Tuberculosis (TB), measles (rubeola), and varicella (chickenpox, shingles in disseminated form).
Core Requirements:
- Patient Placement: The patient must be placed in an Airborne Infection Isolation Room (AIIR). An AIIR is a single-patient room that is equipped with special air handling and ventilation capacity to maintain negative pressure relative to the surrounding area. The door must be kept closed.
- Personal Protective Equipment (PPE): All healthcare personnel must wear a fit-tested N95 respirator or higher-level respiratory protection before entering the room. The respirator must be donned before entry and doffed after exiting. - Patient Transport: Strictly limit patient movement. If transport is essential, the patient must wear a surgical mask to minimize the dispersal of droplet nuclei.
- Personnel Restrictions: Susceptible healthcare personnel should not enter the room of patients with measles or varicella if other immune personnel are available.
Protective Environment (Reverse Isolation)
Distinct from the precautions above, a Protective Environment is designed to protect severely immunocompromised patients (e.g., allogeneic hematopoietic stem cell transplant recipients) from acquiring opportunistic infections from the environment. This involves placing the patient in a room with positive pressure ventilation, HEPA filtration of incoming air, and strict adherence to hand hygiene and cleaning protocols. It is designed to keep pathogens *out* of the patient's room, a reversal of the negative pressure concept used for Airborne Precautions.
The Psychosocial Impact of Isolation
While medically necessary, isolation can have significant negative psychological effects on patients. Feelings of loneliness, depression, anxiety, and even anger are common. Patients may feel stigmatized or neglected. It is a critical nursing and administrative responsibility to mitigate these impacts. Strategies include:
- Clear Communication: Explain the reason for isolation clearly and compassionately. Provide regular updates.
- Facilitating Connection: Encourage communication with family and friends through phone calls or video chats.
- Increasing Staff Contact: While minimizing unnecessary entry, ensure that staff who do enter the room spend quality time addressing the patient's needs, both medical and emotional.
- Providing Stimuli: Offer books, magazines, tablets, or other forms of entertainment to combat boredom and loneliness.
Example: Applying Droplet Precautions
Scenario: A 65-year-old male patient presents to the emergency department with a sudden onset of fever, cough, sore throat, and myalgia. An initial rapid test is positive for Influenza A.
- Initial Action: The patient is immediately given a surgical mask to wear and is moved to a private examination room. This is part of respiratory hygiene/cough etiquette.
- Admission Protocol: The admitting physician orders Droplet Precautions in addition to Standard Precautions.
- Room Placement: The patient is admitted to a private room on the medical floor. A sign indicating "Droplet Precautions" is placed on the door.
- Staff Protocol: Before entering the room, nurses, doctors, and other staff don a surgical mask. They perform hand hygiene and use other PPE (gloves, gown) as needed per Standard Precautions for specific tasks like suctioning.
- Visitor Education: The patient's family is educated on the need to wear a mask inside the room and to perform hand hygiene before leaving. Visits are kept brief.
- Transport: When the patient needs to go for a chest X-ray, he is required to wear a surgical mask during transport and in the imaging department. The transport staff is notified of his precaution status.
This systematic application of Droplet Precautions contains the influenza virus, protecting other vulnerable patients and staff from infection.
Transmisson Precautions Posters
Did You Know?
The concept of separating the sick from the healthy is ancient, but one of the most famous historical cases of isolation involved Mary Mallon, better known as "Typhoid Mary." In the early 1900s, Mallon was an asymptomatic carrier of Salmonella typhi. As a cook, she unknowingly infected dozens of people, leading to several deaths. Because she did not feel sick, she refused to believe she was the source. Public health officials eventually had to forcibly isolate her on North Brother Island in New York, where she spent most of the rest of her life. Her case highlighted the complex public health challenge of managing asymptomatic carriers and the ethical dilemmas surrounding involuntary isolation.
Section 1 Summary
- Isolation protocols interrupt the chain of infection, primarily at the 'mode of transmission' link.
- Standard Precautions are the foundation of infection control, applied universally to all patients.
- Transmission-Based Precautions are used in addition to Standard Precautions for specific pathogens and are categorized into Contact, Droplet, and Airborne.
- Contact Precautions require a gown and gloves and are for diseases spread by touch (e.g., MRSA, C. diff).
- Droplet Precautions require a surgical mask and are for diseases spread by large respiratory droplets (e.g., influenza).
- Airborne Precautions require an N95 respirator and an AIIR (negative pressure room) for diseases spread by tiny airborne particles (e.g., TB, measles).
- Healthcare providers must also address the significant psychosocial needs of patients in isolation.
Reflective Questions
- How would you manage a situation where a patient with dementia, who requires Contact Precautions, repeatedly leaves their room and wanders the hallway? What are the key safety and ethical considerations?
- A patient is diagnosed with active pulmonary tuberculosis (requiring Airborne Precautions) and also has a C. difficile infection (requiring Contact Precautions). What is the correct sequence for donning and doffing the full set of required PPE?
- Consider the psychosocial impact of long-term isolation (e.g., for a patient with multidrug-resistant TB). What innovative strategies could your unit implement to improve the patient's quality of life without compromising safety?
Section 2: Quarantine Procedures in Healthcare Settings
Defining the Distinction: Isolation vs. Quarantine
While often used interchangeably in lay language, "isolation" and "quarantine" have precise and distinct meanings in public health and infection control. As we established in the previous section, isolation separates sick people with a contagious disease from people who are not sick. In contrast, quarantine separates and restricts the movement of people who were exposed to a contagious disease to see if they become sick. These are individuals who are not yet symptomatic but have a high-risk exposure history. The purpose of quarantine is to prevent the spread of disease during the incubation period, the time between exposure and the potential onset of symptoms, when a person might be contagious.
Understanding this difference is paramount for hospital administrators and clinical staff. An isolation order is based on a confirmed or strongly suspected diagnosis. A quarantine order is based on exposure risk and epidemiological linkage. Implementing a quarantine within a hospital setting is a complex operation with significant logistical, ethical, and legal dimensions that must be carefully managed (World Health Organization, 2020).
Legal and Ethical Framework for Quarantine
The authority to enforce quarantine stems from public health law, designed to protect the population from communicable disease threats. However, this authority must be balanced with individual rights and civil liberties. Quarantine is a significant infringement on personal freedom, and as such, it must adhere to key ethical principles:
- Proportionality: The restrictions imposed must be proportional to the public health threat. A highly transmissible and severe disease may warrant more stringent measures than a less severe one.
- Necessity: Quarantine should only be used when it is necessary to protect public health and there are no less restrictive means available to achieve the same goal. For example, if active monitoring of symptoms is sufficient, a full quarantine may not be necessary.
- Scientific Basis: The decision to quarantine, the duration of the quarantine period, and the specific restrictions must be based on the best available scientific evidence about the pathogen's incubation period and mode of transmission.
- Transparency and Fairness: The process should be transparent. Those subject to quarantine must be informed of the reasons, their rights, and have access to a fair process to challenge the order. The application of quarantine should not be discriminatory.
- Humane Treatment: Individuals in quarantine must be treated humanely. Their basic needs—food, water, shelter, and access to medical care and communication—must be met. The psychological toll must also be acknowledged and addressed.
In a hospital, these principles apply to both patients and staff who may be subject to quarantine following a significant exposure event.
Implementing Quarantine Within a Hospital
A quarantine situation in a hospital is typically triggered by an exposure event, such as the discovery that a patient or staff member was unknowingly infectious with a highly contagious disease (e.g., measles, COVID-19) and had contact with others before being placed in appropriate isolation. The response must be swift, systematic, and coordinated by the hospital's infection control department and leadership.
Step 1: Exposure Investigation and Risk Assessment
The first step is to conduct a rapid and thorough epidemiological investigation. This involves:
- Contact Tracing: Identifying every patient, staff member, and visitor who had significant contact with the index case during their infectious period.
- Defining Exposure: Establishing clear criteria for what constitutes a "high-risk" exposure based on the pathogen (e.g., time spent in the same room, proximity, type of interaction, PPE used).
- Assessing Immunity: Determining the immune status of exposed individuals (e.g., vaccination records for measles, prior infection for varicella). Non-immune individuals are at the highest risk.
Step 2: Implementing Quarantine Measures for Patients
For exposed patients who are not immune and must remain in the hospital for other medical reasons, quarantine must be implemented.
- Cohort Quarantine: The most common approach is to implement quarantine for the entire affected ward or unit. Movement in and out of the unit is strictly controlled. Exposed patients are cohorted together, separate from unexposed patients.
- In-Room Quarantine: Patients are confined to their rooms. The door may be kept closed, and Transmission-Based Precautions may be initiated as if they were infectious, especially as the incubation period progresses.
- Symptom Monitoring: Patients in quarantine must be actively monitored for symptoms of the disease, typically at least once or twice a day. This includes temperature checks and screening for specific clinical signs.
- Testing: Depending on the disease, periodic testing may be part of the quarantine protocol to detect infection before symptoms develop.
Step 3: Managing Exposed Healthcare Workers
Quarantining healthcare workers presents a significant challenge due to staffing implications. Policies must be clear and pre-defined.
- Furlough/Home Quarantine: For high-risk exposures, particularly with diseases like measles or Ebola, staff may be furloughed and required to quarantine at home. They must monitor for symptoms and report daily to occupational health. - Work Restrictions: In some cases, asymptomatic but exposed staff may be permitted to work under specific restrictions. This could include being cohorted to care only for the exposed patient cohort, wearing a mask at all times in the facility, and undergoing enhanced symptom monitoring. This decision depends on the pathogen, the nature of the exposure, and the criticality of the staffing situation (Barra et al., 2021).
Step 4: Duration and Discontinuation of Quarantine
The duration of quarantine is determined by the known incubation period of the specific pathogen. It is calculated from the last known exposure and typically extends for the full length of the maximum known incubation period. For example, the quarantine period for measles is 21 days. Quarantine is only lifted after this period has passed without the individual developing symptoms.
Communication: The Critical Element
During a quarantine event, clear, consistent, and empathetic communication is essential to prevent panic and ensure compliance. Hospital leadership must communicate with:
- Patients and Families: Explain why the quarantine is necessary, what to expect, the duration, and how their medical care will continue. Address their fears and concerns.
- Staff: Provide clear instructions on protocols, work restrictions, and symptom monitoring. Offer psychological support, as being part of a quarantine event is highly stressful.
- The Public and Media: A designated spokesperson should provide accurate and timely information to prevent misinformation and maintain public trust in the institution.
Example: Managing a Measles Exposure on a Pediatric Ward
Scenario: A 5-year-old child admitted for a fever of unknown origin develops a classic maculopapular rash and is diagnosed with measles. An investigation reveals the child was in a 4-bed bay on the general pediatric ward for 48 hours while infectious before the diagnosis was made and Airborne Precautions were initiated.
- Investigation: Infection control immediately identifies the 3 other patients in the bay, their parents, and the 12 nurses and 3 physicians who provided care during the 48-hour period.
- Risk Assessment: Vaccination records are checked. One of the exposed patients is a 6-month-old infant too young for the MMR vaccine. Two of the nurses are found to have non-protective antibody titers.
- Patient Quarantine: The entire pediatric ward is closed to new admissions. The exposed, non-immune infant is placed in a private room under quarantine with Airborne Precautions, as they are at high risk of developing the disease. The other exposed patients with documented immunity are monitored for symptoms but may not require strict quarantine.
- Staff Quarantine: The two non-immune nurses are furloughed and instructed to quarantine at home for 21 days from their last exposure. They must perform twice-daily temperature checks. Post-exposure prophylaxis (vaccine or immunoglobulin) is offered.
- Communication: The hospital's Chief Medical Officer holds a meeting with the parents of all patients on the ward to explain the situation. A memo is sent to all hospital staff, and a press release is prepared to inform the public.
Did You Know?
The term "quarantine" originates from the 14th-century Venetian practice of requiring ships arriving from plague-affected ports to anchor for 40 days before landing. This practice, called quarantena (Italian for "forty days"), was based on the observation that this period was long enough to see if the disease would manifest among the crew. While not based on a modern understanding of incubation periods, it was one of the first organized, systematic public health measures and proved to be remarkably effective in slowing the spread of the Black Death into the city-state.
Section 2 Summary
- Isolation is for sick individuals, while quarantine is for healthy individuals who were exposed.
- Quarantine aims to prevent disease spread during the pathogen's incubation period.
- The implementation of quarantine must be guided by strong legal and ethical principles, including necessity, proportionality, and humane treatment.
- In-hospital quarantine involves rapid exposure investigation, cohorting of patients, managing exposed staff through furlough or work restrictions, and active symptom monitoring.
- The duration of quarantine is determined by the maximum incubation period of the specific infectious agent.
- Clear and transparent communication with all stakeholders is crucial for the successful management of a quarantine event.
Reflective Questions
- During a major outbreak, a hospital faces a critical staffing shortage. An asymptomatic nurse has a high-risk exposure to the pathogen. What ethical frameworks would you use to decide whether to have the nurse quarantine at home (protecting patients) versus continue working under restrictions (maintaining care capacity)?
- How can a hospital administration proactively plan for a quarantine event to minimize logistical chaos? What are the top three items that should be in a "Quarantine Preparedness Plan"?
- Imagine you are the nurse manager of a unit placed under quarantine. What are your first steps to address the fear and anxiety of both your staff and the patients on your ward?
Section 3: Air Ventilation and Engineering Controls
The Unseen Protector: The Role of Ventilation
While PPE and hand hygiene are critical behavioral interventions, engineering controls form the physical foundation of a safe environment for managing infectious diseases, particularly those that are airborne. Air ventilation is perhaps the most important engineering control in this context. Its primary purpose is to control the concentration of airborne infectious particles (droplet nuclei) in the air, thereby reducing the risk of transmission to susceptible individuals. The strategy is not to create a completely sterile air environment, but to manage the air in a way that directs contaminants away from people and reduces their concentration to a level where the risk of infection is acceptably low. The American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE) provides critical standards that, along with CDC guidelines, inform hospital ventilation design (ASHRAE, 2021).
The core principles of air ventilation control are:
- Dilution: Introducing clean, outdoor air into a space to dilute the concentration of indoor contaminants.
- Filtration: Removing particles from the air by passing it through a filter. The most common and effective type in healthcare is the HEPA filter.
- Pressure Differentials: Using air pressure to control the direction of airflow between adjacent areas, either containing contaminated air within a room or protecting a room from outside contaminants.
- Source Control/Exhaust: Capturing and removing contaminated air at its source, often by exhausting it directly to the outside.
Airborne Infection Isolation Rooms (AIIRs): A Deep Dive
The AIIR is the specialized patient room required for patients under Airborne Precautions (e.g., TB, measles). It is meticulously engineered to contain airborne pathogens within the room and prevent their escape into adjacent hallways and hospital areas.
1. Negative Pressure
The defining feature of an AIIR is negative pressure. This means the air pressure inside the room is kept lower than the pressure in the surrounding corridor. This differential is achieved by exhausting more air from the room than is supplied to it. Because air naturally flows from areas of higher pressure to lower pressure, this ensures that when the door is opened, clean air from the hallway flows *into* the room, and contaminated air from inside the room is prevented from flowing *out*. This is the critical containment mechanism. The pressure differential is small but sufficient to direct airflow, typically around -2.5 Pascals (-0.01 inches of water gauge).
2. Air Changes Per Hour (ACH)
This metric measures how many times the total volume of air in a room is replaced in one hour. A higher ACH means faster dilution and removal of airborne contaminants. CDC and ASHRAE guidelines mandate a minimum of 12 ACH for new or renovated AIIRs. This high rate of air exchange is crucial for rapidly clearing infectious particles from the air. For example, with 12 ACH, over 99% of airborne contaminants are removed in approximately 23 minutes, and 99.9% are removed in 35 minutes. This calculation is vital for determining how long a room must remain empty after an infectious patient is discharged before it is safe for the next patient to enter (a process known as terminal cleaning and air clearance).
3. Exhaust and HEPA Filtration
The air exhausted from an AIIR must be managed safely. There are two primary methods:
- Direct Exhaust to the Outdoors: The preferred method is to exhaust all air from the room directly to the outside, away from air intakes and populated areas. The dilution effect of the atmosphere renders the exhausted air non-infectious.
- Recirculation through HEPA Filtration: If direct exhaust is not feasible (e.g., in a building where routing ducts outside is impossible), the air can be recirculated back into the main ventilation system, but *only after* it has passed through a High-Efficiency Particulate Air (HEPA) filter. A HEPA filter is a specialized mechanical filter that is rated to remove at least 99.97% of airborne particles 0.3 micrometers (µm) in diameter. This size is chosen because it is the most difficult particle size to capture; the filter is even more efficient at capturing particles that are smaller or larger. This effectively sterilizes the air before it is returned to circulation.
Protective Environments (PEs): The Opposite Principle
For severely immunocompromised patients, the goal is reversed. A Protective Environment (PE) room is engineered to protect the patient from common environmental pathogens. This is achieved through:
- Positive Pressure: The room is maintained at a higher pressure than the surrounding corridor. More clean, filtered air is supplied to the room than is exhausted. When the door is opened, air flows *out* of the room, preventing contaminated air from the hallway (carrying fungi like Aspergillus or other pathogens) from entering.
- HEPA Filtration of Supply Air: All air entering the PE room must first pass through a HEPA filter to remove potential pathogens.
- High ACH: PEs also require a high rate of air exchange (≥12 ACH) to keep the room air as clean as possible.
It is critically important that staff understand the difference between these two room types. Placing an infectious tuberculosis patient in a positive pressure room would be a catastrophic failure of infection control, as it would actively pump contaminated air out into the hospital.
Monitoring and Maintenance: Ensuring System Integrity
An advanced ventilation system is only effective if it is functioning correctly. Rigorous monitoring and maintenance are non-negotiable.
- Daily Monitoring: Nursing staff should perform a simple daily check to verify negative pressure. This can be done by observing a wall-mounted pressure monitor (manometer) which should show a negative reading. A low-tech method is the "tissue test": hold a tissue at the bottom of the door, and it should be pulled inward toward the room.
- Regular Maintenance: Hospital engineering or facilities management must conduct regular inspections, filter changes, and pressure testing as part of a preventive maintenance schedule. Alarms should be in place to alert staff to any system failures.
- Surge Capacity Planning: In an outbreak, the demand for AIIRs can exceed supply. Hospitals must have plans for surge capacity, which may involve using portable HEPA filtration units with exhaust ducting to create temporary negative pressure environments in standard rooms. While not a perfect substitute for a fully engineered AIIR, these units can be a life-saving measure.
Example: Daily AIIR Functionality Check
Scenario: Nurse Sarah is starting her shift and is assigned to a patient with confirmed measles in AIIR Room 402.
- Check the Signage: She first confirms the "Airborne Precautions" and "Negative Pressure Room" signs are clearly posted on the door.
- Check the Monitor: Beside the door is a digital pressure monitor. She observes the reading. The screen shows "-3.0 Pa". This is within the acceptable range (e.g., -2.5 Pa or more negative), confirming that the room is under negative pressure.
- Perform Visual Check (Tissue Test): As a secondary check, she cracks the door open slightly and holds a facial tissue near the bottom opening. The tissue is immediately pulled inward into the room, providing a visual confirmation of the correct directional airflow.
- Don PPE: Having confirmed the room's safety systems are functional, she performs hand hygiene and dons her fit-tested N95 respirator.
- Enter and Close Door: She enters the room, ensuring the door closes firmly behind her to maintain the negative pressure seal.
If at step 2 or 3 the monitor read "0.0 Pa" or the tissue was pushed outward, Sarah would not enter the room. She would keep the door closed, notify the charge nurse and the engineering department immediately, and move the patient's care cart away from the door to prevent staff from entering until the issue is resolved.
Did You Know?
Long before the germ theory of disease was understood, Florence Nightingale was a staunch advocate for the healing power of fresh air. During the Crimean War in the 1850s, she observed that soldiers in crowded, poorly ventilated wards had much higher mortality rates. She insisted on opening windows to improve airflow, a practice she called "natural ventilation." Her meticulous data collection showed a dramatic drop in death rates in the wards she managed. These "Nightingale Wards," large, open rooms with high ceilings and opposing windows, were a precursor to our modern understanding of how dilution ventilation can reduce the transmission of disease.
Section 3 Summary
- Engineering controls, particularly air ventilation, are a critical layer of protection against airborne pathogens.
- Airborne Infection Isolation Rooms (AIIRs) use negative pressure to contain infectious particles within the room, preventing their escape. Air flows from the hallway into the room.
- AIIRs require a high rate of Air Changes per Hour (ACH) (≥12) to dilute and remove contaminants quickly.
- Exhausted air from an AIIR must either be vented directly outside or recirculated only after passing through a HEPA filter.
- Protective Environments (PEs) use positive pressure to protect immunocompromised patients, pushing air from the room out into the hallway to keep pathogens out.
- Daily monitoring (e.g., checking pressure monitors, tissue test) and regular engineering maintenance are essential to ensure these specialized rooms are functioning correctly.
Reflective Questions
- Your hospital is over 50 years old and has very few engineered AIIRs. A pandemic of a novel airborne virus begins. As a member of the infection control committee, what are the top three strategies you would propose to rapidly increase your hospital's capacity to care for patients requiring airborne isolation?
- An electrician needs to enter an occupied AIIR to repair a faulty power outlet. What specific instructions and precautions must you provide to ensure the safety of the electrician and the integrity of the isolation environment?
- During a power outage, the hospital's ventilation system fails. You have a patient with active tuberculosis on the unit. What are your immediate actions to mitigate the risk of transmission to staff and other patients?
Glossary of Key Terms
- Airborne Infection Isolation Room (AIIR)
- A single-patient room with special ventilation to maintain negative pressure, used for patients with diseases transmitted by airborne droplet nuclei (e.g., tuberculosis).
- Air Changes per Hour (ACH)
- A measure of the air ventilation rate in a room; the number of times the total volume of air in a room is replaced each hour.
- Cohort
- The practice of grouping patients infected or colonized with the same organism, or who have had the same exposure, in the same room or area to confine their care to one location.
- HEPA Filter
- High-Efficiency Particulate Air filter capable of removing at least 99.97% of airborne particles 0.3 micrometers in diameter.
- Isolation
- The separation of a person or group of people known or reasonably believed to be infected with a communicable disease from those who are not infected to prevent spread.
- Negative Pressure
- An engineering control where the air pressure inside a room is lower than the air pressure outside of it, causing air to flow into the room and preventing airborne particles from escaping.
- Positive Pressure
- An engineering control where the air pressure inside a room is higher than the air pressure outside of it, causing air to flow out of the room and preventing airborne particles from entering.
- Quarantine
- The separation and restriction of movement of a person or group of people who are not yet ill but have been exposed to a communicable disease, to see if they become ill.
- Standard Precautions
- The minimum infection prevention practices that apply to all patient care, regardless of suspected or confirmed infection status.
- Transmission-Based Precautions
- A second tier of infection control practices used in addition to Standard Precautions for patients with known or suspected infections that are spread by contact, droplet, or airborne routes.
References
American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE). (2021). Standard 170-2021: Ventilation of health care facilities. ASHRAE.
Barra, L., Smith, M., & Pineles, L. (2021). Risk of infection to healthcare workers following unprotected exposure to a patient with COVID-19. Infection Control & Hospital Epidemiology, 42(3), 356–358.
Centers for Disease Control and Prevention. (2016). Core infection prevention and control practices for safe healthcare delivery in all settings – recommendations of the Healthcare Infection Control Practices Advisory Committee. Retrieved from https://www.cdc.gov/hicpac/recommendations/core-practices.html
Siegel, J. D., Rhinehart, E., Jackson, M., Chiarello, L., & Health Care Infection Control Practices Advisory Committee. (2007). 2007 Guideline for isolation precautions: Preventing transmission of infectious agents in health care settings. Centers for Disease Control and Prevention.
World Health Organization. (2020). Considerations for quarantine of individuals in the context of containment for coronavirus disease (COVID-19). WHO/2019-nCoV/IHR_Quarantine/2020.3.